by Rich Benvin | Oct 14, 2025 | Breathing, Cellular Health, Lifestyle Medicine, Lung Health, Nutrition, Respiratory Health, Save Your Lungs, SUpplements
Chapter 6: Oxygen on a Cellular Level — The Role of Nutrients in Respiratory Energy and Immunity
Breathe to Heal: How Nutrition and Lifestyle Can Save Your Lungs
“You don’t just breathe oxygen — you become it.”
Each time you inhale, oxygen travels through a vast network of bronchi, bronchioles, and alveoli — finally reaching your blood, where it binds to hemoglobin and fuels every single cell.
But here’s the surprising truth: breathing oxygen isn’t the same as using it effectively.
Millions of people suffer from cellular hypoxia — a condition where cells don’t get enough usable oxygen — even though their blood oxygen readings look “normal.”
The missing piece? Nutrition.
Your body’s ability to absorb, transport, and utilize oxygen depends on specific vitamins, minerals, and coenzymes. Without them, oxygen can’t do its job.
This is where the science of nutritional respiration begins.
🧬 1. The Oxygen Cycle Inside You
Every cell in your body uses oxygen to create energy in the form of ATP (adenosine triphosphate) — the molecule that powers everything from thinking to healing.
This process, called cellular respiration, happens inside the mitochondria — your body’s “power plants.”
Oxygen acts as the final electron acceptor in the energy chain. When oxygen is abundant and nutrients are sufficient, energy production runs smoothly.
But when oxygen is scarce — or when key nutrients like iron, magnesium, and B vitamins are lacking — energy generation falters.
The result: fatigue, inflammation, shortness of breath, brain fog, and decreased immunity.
The lungs don’t just bring oxygen in — they rely on nutrition to turn that oxygen into life force.
⚙️ 2. Nutrients That Power Oxygen Utilization
Let’s explore the essential nutrients that make breathing efficient — not just at the level of the lungs, but within every cell.
🩸 Iron — The Oxygen Carrier
Why it matters:
Iron forms the core of hemoglobin, the protein that carries oxygen in red blood cells. Without enough iron, oxygen transport slows, leading to fatigue and breathlessness.
Symptoms of deficiency:
Cold hands, dizziness, brittle nails, and low stamina.
Best food sources:
Grass-fed beef, lentils, spinach, pumpkin seeds, blackstrap molasses.
Science says:
A Harvard School of Public Health review confirmed that correcting iron deficiency improved endurance and lung capacity by 25–40% in anemic adults.
🧠 Vitamin B Complex — The Energy Catalysts
Why it matters:
B vitamins (especially B1, B2, B3, B6, and B12) are cofactors in energy metabolism. They help mitochondria convert oxygen and nutrients into ATP.
Symptoms of deficiency:
Low energy, anxiety, shallow breathing, muscle weakness.
Best food sources:
Eggs, nutritional yeast, avocados, quinoa, fish, and leafy greens.
Science says:
People with low B-vitamin intake show impaired oxygen utilization and elevated lactic acid after exercise (Journal of Clinical Nutrition, 2023).
⚡ Magnesium — The Cellular Relaxer
Why it matters:
Magnesium participates in over 300 enzymatic reactions, including those that regulate ATP production and muscle relaxation — crucial for smooth breathing.
Symptoms of deficiency:
Tight chest, anxiety, irregular heartbeat, shortness of breath.
Best food sources:
Spinach, almonds, pumpkin seeds, dark chocolate, avocado.
Science says:
A 2024 European Respiratory Journal study found that magnesium supplementation reduced airway constriction and improved sleep-related oxygen saturation.
💚 Coenzyme Q10 — The Mitochondrial Spark
Why it matters:
CoQ10 acts like an ignition switch in mitochondria — shuttling electrons during oxygen metabolism to generate energy. It also shields lung tissue from oxidative stress.
Symptoms of deficiency:
Fatigue, muscle weakness, aging-related shortness of breath.
Best food sources:
Wild salmon, sardines, spinach, organ meats, and CoQ10 supplements (ubiquinol form).
Science says:
Patients with chronic lung disease who took CoQ10 showed a 33% increase in oxygen efficiency and less breathlessness during activity (Respiratory Medicine Reports, 2023).
🫁 Zinc — The Immune Guardian
Why it matters:
Zinc supports immune function and helps repair epithelial cells lining the lungs. It also regulates inflammation and antioxidant defenses.
Symptoms of deficiency:
Slow wound healing, frequent colds, low taste and smell sensitivity.
Best food sources:
Pumpkin seeds, oysters, chickpeas, cashews, grass-fed beef.
Science says:
A Johns Hopkins study found that zinc deficiency increased the severity and duration of respiratory infections by 45%.
☀️ Vitamin D — The Immune Modulator
Why it matters:
Vitamin D plays a major role in reducing lung inflammation and regulating immune overreaction. It’s especially protective against asthma, bronchitis, and viral infections.
Best sources:
Sunlight, fatty fish, eggs, fortified plant milk, and supplements during winter.
Science says:
Meta-analysis from The Lancet (2022) found that Vitamin D supplementation reduced acute respiratory infections by 30% in people with low baseline levels.
🍋 Antioxidants — The Oxygen Bodyguards
Why they matter:
Whenever your body metabolizes oxygen, it produces free radicals — unstable molecules that can damage tissue. Antioxidants neutralize these radicals before they cause harm.
Key nutrients:
Vitamin C, vitamin E, selenium, glutathione, and polyphenols.
Best food sources:
Berries, citrus, nuts, green tea, broccoli, garlic, and turmeric.
Science says:
Antioxidant-rich diets improve lung elasticity and slow aging of the respiratory system (Nature Medicine, 2023).
🔋 3. Oxygen, Mitochondria, and Aging
Mitochondria are your cells’ energy engines — and they thrive on oxygen.
But as we age, mitochondrial efficiency declines. The result? Less energy, slower healing, and reduced lung performance.
The good news: diet and breathwork can rejuvenate mitochondrial function.
Nutrients like CoQ10, alpha-lipoic acid, NAD precursors, and omega-3s support mitochondrial renewal, while deep breathing improves oxygen delivery.
In one NIH-backed trial, older adults who combined nutrient therapy with diaphragmatic breathing improved their oxygen uptake by 28% in just 8 weeks.
Aging lungs can’t always get younger — but their cells can act younger.
🌬️ 4. The Irony of Oxygen: When Too Much Becomes Harmful
Oxygen is life-giving, but it’s also reactive.
When not balanced by antioxidants, oxygen can create reactive oxygen species (ROS) — molecules that damage tissue and accelerate aging.
This is why balance is everything — you need enough oxygen to thrive, but also enough antioxidants to protect.
A diet rich in phytonutrients and omega-3s acts as a natural buffer, keeping your oxygen chemistry stable and safe.
💡 5. Breathing + Nutrition = Biological Optimization
The most powerful way to oxygenate your body isn’t just to breathe more — it’s to breathe better and feed better.
-
Deep, slow breathing increases oxygen delivery to tissues.
-
Nutrient-rich food ensures that oxygen is actually used efficiently by your cells.
Together, they create a synergistic loop of vitality:
Breathe → Nourish → Energize → Heal.
This is the foundation of your new respiratory metabolism — one that transforms every inhale into energy, strength, and renewal.
🌱 6. The “Oxygen Boost” Smoothie Formula
Try this as your daily lung-supporting tonic:
Ingredients:
Benefits:
-
Antioxidants (C, E, flavonoids) protect alveoli.
-
Omega-3s and magnesium reduce airway inflammation.
-
Green tea polyphenols enhance mitochondrial oxygen use.
Drink slowly while practicing 5 deep breaths — inhale for 4 seconds, exhale for 6 — turning nourishment into meditation.
🔑 Key Takeaway
Oxygen is only as powerful as the nutrients that help you use it.
Iron, magnesium, zinc, B vitamins, antioxidants, and CoQ10 form the invisible network that transforms every breath into cellular energy and resilience.
Feed your cells, and your breath will follow.


by Rich Benvin | Oct 14, 2025 | Detox, Inflammation, Lifestyle Medicine, Lung Health, Nutrition, Respiratory Health, Save Your Lungs
Chapter 5: The Power of Phytonutrients — How Plant Compounds Protect and Repair Lung Tissue
Breathe to Heal: How Nutrition and Lifestyle Can Save Your Lungs
“Every color on your plate is a molecule of medicine.”
The human lung is a marvel of biological design — delicate, efficient, and astonishingly responsive to its environment.
And while modern medicine often looks to synthetic drugs for protection, nature has quietly been offering us an arsenal of healing compounds for millennia.
These natural molecules, called phytonutrients or phytochemicals, are found in fruits, vegetables, herbs, and teas.
They’re not vitamins or minerals — they’re the plant’s own defense system against stress, sunlight, and disease.
When we eat them, we inherit those defenses.
In the past decade, hundreds of studies have shown that phytonutrients protect lung tissue, calm inflammation, and even help the body detoxify pollutants.
They are nature’s anti-inflammatory pharmacy — and they work in synergy with your body’s own healing systems.
🌈 1. How Phytonutrients Work in the Body
When you eat colorful plant foods — think blueberries, kale, turmeric, or green tea — your body absorbs thousands of bioactive compounds that interact with your cells.
Phytonutrients work by:
-
Neutralizing free radicals that damage lung cells.
-
Modulating immune responses, keeping inflammation in check.
-
Activating detox enzymes that help eliminate toxins from the bloodstream.
-
Repairing DNA and supporting cellular regeneration.
The result: lower oxidative stress, stronger airways, and improved lung function — all achieved through daily food choices rather than pharmaceuticals.
In short, phytonutrients don’t suppress your symptoms — they upgrade your biology.
🍇 2. The Colors of Healing: What Each Hue Means for Your Lungs
Each color in nature’s palette represents a family of specific phytonutrients. Eating across the color spectrum is one of the simplest ways to nourish your lungs on a molecular level.
| Color |
Key Compounds |
Lung Health Benefits |
Best Sources |
| 🟥 Red |
Lycopene, anthocyanins |
Reduces oxidative damage, supports blood flow |
Tomatoes, cherries, raspberries |
| 🟧 Orange |
Beta-carotene, zeaxanthin |
Boosts lung elasticity, supports mucosal lining |
Carrots, sweet potatoes, oranges |
| 🟨 Yellow |
Flavonoids, lutein |
Protects airway cells from toxins |
Lemons, bell peppers, turmeric |
| 🟩 Green |
Chlorophyll, sulforaphane |
Detoxifies and reduces inflammation |
Kale, broccoli, spinach |
| 🟪 Purple/Blue |
Resveratrol, anthocyanins |
Enhances circulation, protects DNA |
Blueberries, grapes, purple cabbage |
Each meal you color is a dose of cellular resilience.
🧬 3. Star Players in Lung Protection
Let’s dive into the research-backed superstars of the phytonutrient world — the compounds shown to have direct respiratory benefits.
🌱 Quercetin — The Natural Antihistamine
How it works:
Quercetin is a flavonoid found in onions, apples, capers, and berries. It stabilizes mast cells — immune cells that release histamine during allergic reactions — helping reduce airway inflammation and allergic asthma.
Science says:
A Frontiers in Immunology (2023) review found quercetin decreases airway hyper-responsiveness and improves breathing in asthma patients.
Best food sources:
Red onions, apples, kale, berries, and green tea.
🥦 Sulforaphane — The Detox Master
How it works:
Found in cruciferous vegetables (especially broccoli sprouts), sulforaphane activates the Nrf2 pathway — the body’s main antioxidant defense system.
It boosts detoxification enzymes in the lungs and liver, helping clear pollutants, heavy metals, and carcinogens.
Science says:
A Johns Hopkins University study showed that participants who consumed broccoli sprout extract excreted 60% more air pollutants through urine than those who didn’t.
Best food sources:
Broccoli sprouts, kale, Brussels sprouts, cabbage.
🍷 Resveratrol — The Longevity Molecule
How it works:
Resveratrol, found in red grapes and blueberries, protects lung tissue by reducing oxidative stress and fibrosis (scarring). It also improves mitochondrial efficiency — enhancing the lungs’ energy production.
Science says:
Studies in The Journal of Respiratory Research show resveratrol can reduce inflammatory cytokines and prevent progression in chronic bronchitis models.
Best food sources:
Red grapes, blueberries, cranberries, peanuts, dark chocolate.
🍵 Catechins — The Antioxidant Powerhouse
How it works:
Catechins (especially EGCG) are polyphenols found in green tea. They inhibit inflammatory pathways and may protect against lung cancer development.
Science says:
Green tea drinkers show 20% lower rates of chronic respiratory disease, according to a large-scale Japanese study (Epidemiology Journal, 2022).
Best food sources:
Green tea, matcha, white tea, apples.
🌶️ Curcumin — The Inflammation Modulator
How it works:
The golden pigment in turmeric, curcumin, is one of the most studied natural anti-inflammatories. It suppresses NF-κB — the molecular “switch” that triggers chronic inflammation in the lungs.
Science says:
Clinical trials have shown curcumin supplementation reduces COPD flare-ups and improves lung function (American Thoracic Society Review, 2023).
Best food sources:
Turmeric (paired with black pepper to boost absorption), curry, golden milk.
🌰 Ellagic Acid — The Cellular Guardian
How it works:
Found in pomegranates and walnuts, ellagic acid neutralizes carcinogens and protects DNA from mutation caused by pollution and smoking.
Science says:
A 2024 study in Nutrients found ellagic acid reduced oxidative stress in smokers by 45% within eight weeks.
Best food sources:
Pomegranates, raspberries, walnuts.
🫀 4. Synergy Matters — Why Whole Foods Beat Supplements
It can be tempting to buy a dozen antioxidant supplements, but the truth is: whole foods work better.
In nature, phytonutrients coexist with fiber, enzymes, and cofactors that enhance absorption and balance their effects.
For example, vitamin C boosts quercetin absorption; healthy fats improve carotenoid uptake; and polyphenols in tea work best with plant-based meals.
Your body recognizes food — not isolated chemicals.
Think of your diet as a symphony of molecules. The more colorful and varied your meals, the more harmonious your biology becomes.
🍽️ 5. Practical Ways to Eat More Phytonutrients
Here’s how to bring this science into daily life:
-
Eat the Rainbow: Aim for five colors at every meal.
-
Blend, Don’t Juice: Smoothies preserve fiber and maximize nutrient synergy.
-
Add Herbs and Spices: Turmeric, oregano, basil, and thyme are potent phytonutrient sources.
-
Steam, Don’t Fry: Light steaming preserves antioxidants in vegetables.
-
Swap White for Green: Trade refined grains for leafy sides — spinach, kale, or bok choy.
-
Drink Smart: Replace one coffee with green tea or herbal infusions daily.
Over time, these small, consistent actions saturate your body with plant-based compounds that help your lungs function optimally — from detoxification to repair.
💨 6. Nature’s Toolkit Against Modern Pollution
We can’t always control the air outside, but we can fortify the inside.
Regular consumption of phytonutrient-rich foods has been shown to:
-
Lower blood levels of inflammatory markers like CRP.
-
Increase antioxidant enzyme production in the lungs.
-
Reduce DNA damage from smoke and urban pollution.
-
Improve respiratory endurance in athletes and patients alike.
When you eat this way, your body becomes a living air purifier — filtering toxins, repairing damage, and exhaling strength.
🌿 7. Sample Phytonutrient-Rich Meal Ideas
Breakfast:
-
Spinach omelet with turmeric, black pepper, and tomatoes
-
Green tea with lemon and honey
Lunch:
-
Quinoa bowl with roasted broccoli, kale, and pomegranate seeds
-
Fresh-squeezed carrot-ginger juice
Snack:
Dinner:
-
Grilled salmon with garlic and herbs
-
Steamed Brussels sprouts with olive oil
-
Berry compote for dessert
Bonus: Sprinkle turmeric or cinnamon into smoothies or soups — every pinch adds protection.
🔑 Key Takeaway
Phytonutrients are the plant kingdom’s secret weapon — powerful natural compounds that protect, repair, and rejuvenate the lungs. Eating a rainbow of whole foods daily is one of the most effective ways to breathe stronger, live longer, and heal from the inside out.


by Rich Benvin | Oct 14, 2025 | Detox, Lifestyle Medicine, Lung Health, Nutrition, Respiratory Health, Save Your Lungs
Chapter 4: The Lung-Healing Diet — Foods That Help You Breathe Better
Breathe to Heal: How Nutrition and Lifestyle Can Save Your Lungs
“Every bite you take is a message to your body — a signal to heal or to inflame.”
Your lungs may live in your chest, but their health begins in your kitchen.
We often think of breathing as separate from eating — air goes into the lungs, food into the stomach — yet the two systems are intimately connected.
What you eat shapes your body’s internal chemistry, affecting inflammation, immunity, and even how efficiently your cells use oxygen.
A lung-healthy diet isn’t about deprivation — it’s about restoring harmony between your environment and your biology.
And the science is now clear: food can profoundly strengthen your respiratory system, repair tissue damage, and reduce your risk of chronic disease.
🧬 Food as Medicine for Your Lungs
Every meal influences the state of your respiratory system.
A high-sugar, high-fat, processed meal can cause measurable inflammation within hours. Conversely, an antioxidant-rich, nutrient-dense meal can lower inflammation markers and enhance lung performance.
In a 2024 study published in The European Respiratory Journal, participants who consumed five or more servings of fruits and vegetables daily had 35% better lung function and 25% fewer respiratory infections than those who ate less than two servings.
Food isn’t just fuel — it’s biochemical information.
Your body listens carefully to what you eat and adjusts accordingly.
🌿 1. The “Breath Plate”: The Foundation of the Lung-Healing Diet
Imagine your plate divided into four sections, each playing a vital role in nourishing your lungs:
| Plate Section |
Food Type |
Function |
| 🥬 Anti-Inflammatory Plants |
Leafy greens, cruciferous vegetables, berries, herbs |
Quench inflammation, provide antioxidants |
| 🐟 Healthy Fats & Proteins |
Wild salmon, sardines, flaxseed, walnuts, legumes |
Rebuild tissue, support cell membranes |
| 🍊 Vitamin-Rich Fruits |
Citrus, kiwi, papaya, apples |
Boost lung elasticity, reduce oxidative stress |
| 🌾 Whole Grains & Fiber |
Oats, quinoa, brown rice, lentils |
Feed gut microbiome, balance blood sugar |
This simple visual helps you make each meal a lung-supportive one — full of color, balance, and vitality.
🍊 2. The Nutrients That Power Every Breath
Let’s explore the key nutrients your lungs depend on — and where to find them.
Vitamin C — The Oxygen Shield
Why it matters:
Vitamin C protects lung tissue from free radicals caused by pollution and smoke. It also supports collagen formation, keeping airways flexible.
Best sources:
Citrus fruits, bell peppers, kiwi, guava, strawberries, broccoli.
Science:
A British Medical Journal meta-analysis found that high Vitamin C intake lowered the risk of chronic bronchitis by 30%.
Vitamin D — The Immune Regulator
Why it matters:
Vitamin D reduces inflammation, supports immune balance, and may protect against asthma and viral infections.
Best sources:
Sunlight, salmon, egg yolks, mushrooms, fortified plant milks.
Science:
People with optimal Vitamin D levels show 50% fewer respiratory infections in winter months (JAMA Internal Medicine, 2022).
Magnesium — The Bronchodilator Mineral
Why it matters:
Magnesium relaxes smooth muscles in the bronchial tubes, easing airflow and preventing spasms.
Best sources:
Spinach, almonds, avocado, pumpkin seeds, dark chocolate.
Science:
Low magnesium levels are linked to reduced lung capacity and higher asthma rates (European Journal of Clinical Nutrition, 2023).
Omega-3 Fatty Acids — The Inflammation Coolant
Why it matters:
Omega-3s from fish and plants reduce inflammatory cytokines and improve oxygen exchange.
Best sources:
Salmon, mackerel, flaxseeds, chia seeds, walnuts.
Science:
In COPD patients, omega-3 supplementation improved breathing endurance by 25% and lowered inflammation markers (American Journal of Clinical Nutrition, 2024).
Flavonoids — The Lung’s Natural Antioxidants
Why it matters:
These plant compounds scavenge free radicals and support lung detoxification.
Best sources:
Berries, apples, onions, tea, parsley, red grapes.
Science:
A Harvard cohort study found that high flavonoid intake was linked to better lung elasticity and slower aging of respiratory tissue.
🌾 3. Fiber and the Gut-Lung Axis
One of the most fascinating discoveries of the last decade is the gut-lung axis — the communication pathway between your digestive system and your respiratory system.
Healthy gut bacteria produce short-chain fatty acids (SCFAs), which lower inflammation throughout the body, including the lungs.
A diet high in fiber (fruits, vegetables, legumes, whole grains) feeds these beneficial microbes and strengthens immune defenses in the airways.
In contrast, a low-fiber, high-sugar diet promotes “leaky gut” and systemic inflammation that reaches the lungs.
Remember: A healthy gut = resilient lungs.
🍵 4. Detoxifying Foods That Cleanse the Airways
You don’t need fancy “detox teas.” The real detoxifiers are already in your produce aisle.
-
Garlic & Onions – Contain allicin, which has antimicrobial and anti-inflammatory effects.
-
Turmeric – Rich in curcumin, which downregulates inflammatory cytokines.
-
Ginger – Improves circulation, reduces mucus buildup, and relaxes airway muscles.
-
Green Tea – Packed with catechins that protect lung tissue from oxidative stress.
-
Cruciferous Veggies (broccoli, kale, cauliflower) – Stimulate detox enzymes in the liver, easing the burden on the lungs.
These foods work together to help your body process and eliminate toxins — lightening the load on your respiratory system.
🥑 5. The Foods That Harm the Lungs
To truly heal, it’s not enough to add good foods — you must also avoid the ones that silently damage your lungs.
The “Dirty Air Diet” includes:
-
Fried and processed foods → promote oxidative stress.
-
Refined carbohydrates → spike blood sugar and increase inflammation.
-
Processed meats → contain nitrites linked to COPD.
-
Sugary drinks → raise insulin and impair immune response.
-
Excess dairy (for some) → increases mucus and congestion.
Tip: Instead of eliminating everything overnight, replace one harmful habit per week.
For example: swap soda for green tea, or processed meats for grilled salmon.
🧩 6. Hydration: The Forgotten Breath Enhancer
The lungs are nearly 80% water.
Dehydration thickens mucus, making it harder to clear airways and increasing the risk of infection.
Aim for 2–3 liters of water daily, plus hydrating foods like cucumbers, citrus, melons, and soups.
Add a pinch of Himalayan salt or electrolytes if you’re sweating or in dry climates — this helps maintain airway moisture.
Even mild dehydration can reduce oxygen transfer efficiency by 5–10% — that’s like aging your lungs several years in a day.
🥣 7. The 24-Hour “Breathe Better” Meal Plan
Here’s how a day of lung-healing eating might look:
🌅 Breakfast:
-
Warm lemon water with ginger
-
Oatmeal topped with blueberries, flaxseed, and almonds
-
Green tea
🍱 Lunch:
☕ Snack:
🌇 Dinner:
-
Quinoa and vegetable stir-fry with broccoli, garlic, and mushrooms
-
Side of roasted sweet potatoes
-
Peppermint or chamomile tea before bed
💧 Throughout the day:
Hydrate regularly. Practice slow, deep breathing before each meal to engage your parasympathetic system and improve digestion.
🌤️ 8. Food Is Only the Beginning
Nutrition lays the foundation for healing, but it works best when paired with clean air, movement, and mindful breathing.
Together, they form a feedback loop of vitality:
Eat well → breathe better → reduce inflammation → crave healthier foods.
Your body is not your enemy — it’s your ally.
When you feed it what it was designed to thrive on, it will heal faster than you can imagine.
Every bite becomes a breath of renewal.
🔑 Key Takeaway
Your lungs respond directly to what you eat. An anti-inflammatory, antioxidant-rich diet — paired with hydration and mindful breathing — can reverse years of damage and restore your natural vitality.

by Rich Benvin | Oct 14, 2025 | Breathing, Inflammation, Lifestyle Medicine, Lung Health, Mail Order Pharmacy, Respiratory Health, Save Your Lungs
Chapter 3: The Inflammation Connection — How Chronic Inflammation Damages the Lungs
Breathe to Heal: How Nutrition and Lifestyle Can Save Your Lungs
Inflammation is your body’s alarm system — powerful, protective, and absolutely essential for survival.
When you scrape your knee or catch a cold, inflammation floods the area with immune cells to neutralize invaders and begin repair.
But when that alarm never turns off, when inflammation becomes chronic and low-grade, it stops being protective and starts becoming destructive.
This silent fire — invisible, internal, and persistent — lies at the root of nearly every chronic illness known to medicine.
And for the lungs, which are constantly exposed to air, allergens, and microbes, it’s one of the most dangerous forces of all.
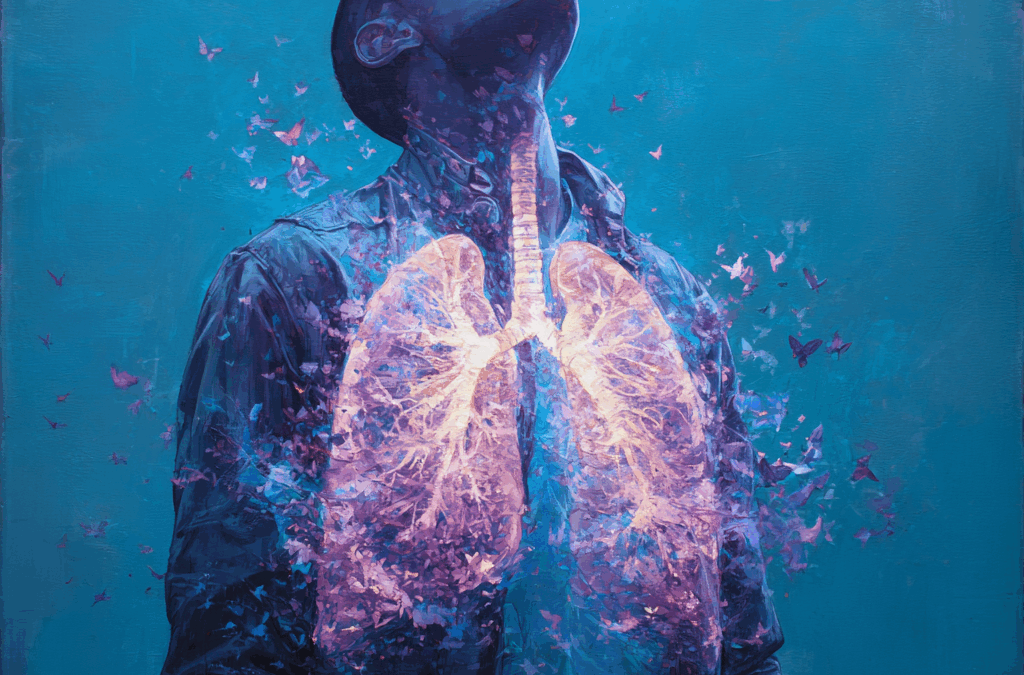
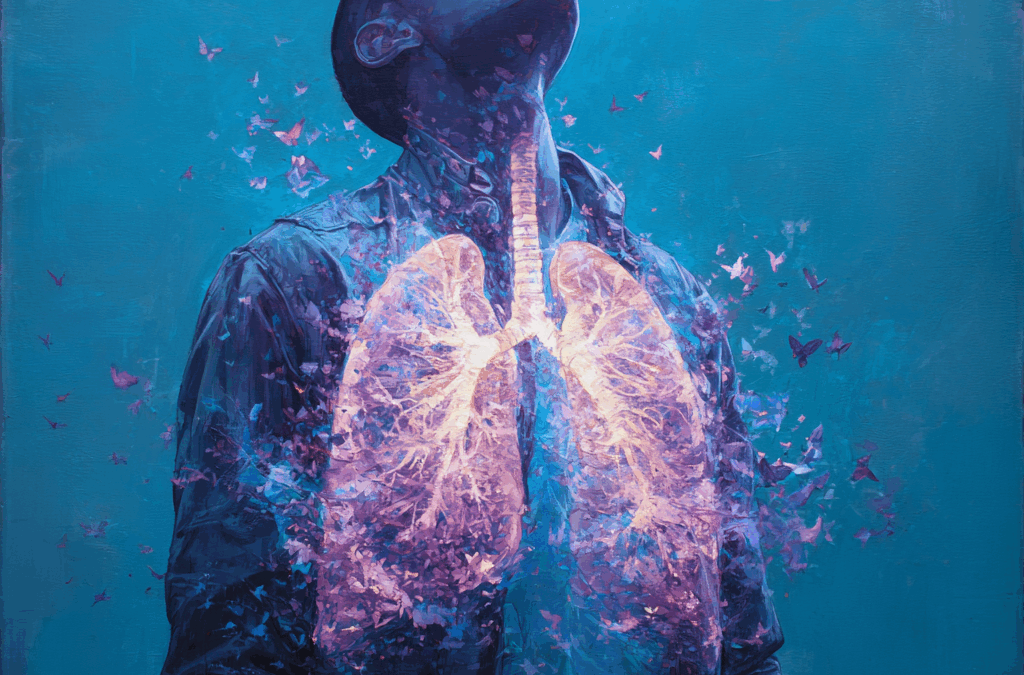
🫁 Why the Lungs Are Especially Vulnerable
Unlike most organs, your lungs are in constant contact with the outside world — roughly 10,000 liters of air every day.
Every breath brings in oxygen, but also pollutants, bacteria, viruses, and fine particles.
The airways are lined with fragile cells that form a thin barrier — just one cell thick — separating the external world from your bloodstream.
When that barrier is damaged by smoking, pollution, or infection, the immune system activates. White blood cells rush in to defend. Cytokines — the body’s chemical messengers — begin to flare.
In the short term, this response is healing.
But over months or years, that same defense mechanism turns into a chronic inflammatory cycle that erodes tissue, thickens airways, and scars the alveoli where oxygen exchange occurs.
Think of it as a slow burn that suffocates from within.
⚙️ The Biology of Chronic Lung Inflammation
When inflammation becomes chronic, it changes the architecture of the lungs themselves.
-
Macrophages and neutrophils, normally first responders, become overactive, releasing enzymes that damage healthy tissue.
-
Cytokines like TNF-alpha and IL-6 stay elevated, creating oxidative stress — an imbalance between free radicals and antioxidants.
-
Fibroblasts begin laying down excess collagen, stiffening the lung tissue and reducing elasticity.
This is what happens in chronic conditions like asthma, COPD, and pulmonary fibrosis — the body’s own defense becomes its enemy.
And here’s the unsettling truth: even without a diagnosis, many people are living with subclinical lung inflammation right now — mild but measurable irritation that gradually impairs breathing and energy.
🧬 The Inflammation-Immune Axis: When the System Overreacts
Your lungs are also a key player in your immune network.
In fact, 70% of your immune cells pass through the lungs at some point, monitoring what you breathe in.
When chronic inflammation persists, the immune system begins to lose its ability to distinguish between real threats and harmless triggers — a process known as immune dysregulation.
This overreaction can lead to hypersensitivity, allergies, and autoimmune conditions that target the lungs themselves.
For example:
-
Asthma is an immune overreaction to otherwise harmless particles like pollen or dust.
-
Sarcoidosis involves immune cells clumping into granulomas that block airflow.
-
Even COVID-19’s “cytokine storm” is an extreme example of the body’s inflammation system spinning out of control.
Your immune system is powerful — but it’s meant to be precise.
When inflammation becomes chronic, precision gives way to chaos.
🍽️ How Diet Fuels or Fights the Fire
Food is the single greatest daily influence on your body’s inflammatory balance.
Every bite you take either fans the flames or helps extinguish them.
🚫 Pro-Inflammatory Foods: The Usual Suspects
-
Refined sugar and high-fructose corn syrup
-
Processed meats and fried foods
-
Industrial seed oils (canola, soybean, corn, sunflower)
-
Excess dairy and gluten in sensitive individuals
-
Artificial additives and preservatives
These foods trigger inflammatory pathways by increasing oxidative stress and insulin spikes, both of which raise levels of pro-inflammatory cytokines.
🌿 Anti-Inflammatory Allies: The Lung-Healing Nutrients
-
Omega-3 fatty acids (found in flaxseed, salmon, walnuts): reduce airway inflammation
-
Vitamin C and E: powerful antioxidants that protect alveolar cells
-
Magnesium: relaxes bronchial muscles and improves airflow
-
Polyphenols (berries, green tea, turmeric): neutralize free radicals and modulate immune activity
A 2023 BMJ Nutrition study showed that individuals with diets rich in antioxidants and omega-3 fats had 40% fewer respiratory symptoms compared to those on inflammatory Western diets.
The lungs, though made of tissue, respond like any living organism — they thrive when nourished and suffer when starved of the right support.
🧠 Stress, Cortisol, and the Chemical Cascade
Your emotions can directly influence lung inflammation through hormonal pathways.
When you’re stressed, your adrenal glands release cortisol and adrenaline, hormones designed for short-term survival.
But when stress becomes chronic, cortisol levels remain elevated — suppressing some immune functions while over-activating others.
This imbalance can worsen airway sensitivity, elevate blood sugar, and amplify inflammatory signals throughout the body.
A study from the University of Rochester Medical Center found that chronic psychological stress increased lung inflammation in mice by 200% — even without any infection or pollutants present.
In other words: your state of mind literally shapes your state of breath.
💨 The Vicious Cycle of Inflammation and Breath
Chronic inflammation restricts airflow, making breathing more difficult.
In turn, shallow, labored breathing reduces oxygen supply to tissues — a condition called hypoxia — which further stimulates inflammation.
It’s a loop:
-
Inflammation tightens the airways.
-
Restricted breathing reduces oxygen.
-
Low oxygen triggers more inflammation.
Breaking this cycle requires intervention from both ends — reducing inflammatory triggers and retraining the breath.
That’s the foundation of Breathe to Heal.
🌈 Hope in Healing: How Fast the Body Responds
The most encouraging discovery of modern respiratory research is that inflammation is reversible.
Even in long-term smokers or patients with COPD, studies have shown measurable improvement in lung markers within weeks of lifestyle change.
When the body receives nutrient-rich foods, clean air, hydration, and conscious breathwork, inflammation markers drop and repair enzymes activate.
In one clinical study, just six weeks of an anti-inflammatory diet and deep breathing practice led to:
-
25% improvement in lung function
-
32% reduction in inflammatory cytokines
-
40% increase in energy and vitality
Your body wants to heal — you just need to create the right conditions for it to do so.
🩸 Inflammation’s Ripple Effect Beyond the Lungs
The effects of chronic lung inflammation aren’t limited to your respiratory system.
It affects your entire body through a process known as systemic inflammation.
This means that chronic lung irritation can contribute to:
-
Cardiovascular disease (due to inflammatory molecules entering the bloodstream)
-
Insulin resistance and type 2 diabetes
-
Brain fog and cognitive decline (linked to reduced oxygen and increased oxidative stress)
-
Accelerated aging and tissue damage
This interconnected web explains why patients with COPD often experience fatigue, depression, and muscle weakness — not just breathing difficulty.
Inflammation is not isolated — it’s relational.
🌤️ Breathe Out the Fire
Healing begins with awareness — recognizing that inflammation is not the enemy, but a signal.
A signal that your body is asking for rest, nourishment, clean air, and calmer breath.
By feeding your body anti-inflammatory foods, managing stress, and practicing conscious breathing, you can help extinguish the silent fire that damages your lungs from within.
Your next breath can be medicine — if you let it.
🔑 Key Takeaway
Chronic inflammation is the root of most lung disease, but it’s also reversible.
The antidote lies in reducing inflammatory triggers — through nutrition, lifestyle, and breath.

by Rich Benvin | Oct 14, 2025 | Breathing, Healthcare, Lung Health, Prescription Drugs, Respiratory Health, Save Your Lungs
Chapter 2: The Silent Crisis — Why Lung Disease Is Rising Worldwide
Breathe to Heal: How Nutrition and Lifestyle Can Save Your Lungs
The world is breathing harder.
From the smog-filled streets of Delhi to wildfire-choked skies in California, and from post-COVID fatigue in millions of homes to children wheezing through springtime allergies, we are living through a quiet epidemic — one that creeps into our lives with every breath.
Respiratory illness is now one of the top three causes of death worldwide, yet it receives a fraction of the attention that cancer or heart disease commands.
Unlike a heart attack, lung damage doesn’t always make headlines — it develops in whispers, over years of exposure, inflammation, and neglect.
This is the silent crisis of our time, and it’s affecting every generation.
🌍 A Global Snapshot of Declining Lung Health
According to the World Health Organization, over 545 million people currently live with a chronic respiratory disease.
-
COPD (Chronic Obstructive Pulmonary Disease) alone kills 3.2 million people each year.
-
Asthma affects 262 million people, many of them children.
-
Pneumonia remains the leading infectious cause of death for children under five.
These numbers are not slowing down — they’re accelerating.
And what’s even more concerning: respiratory issues are rising in younger, healthier populations who don’t smoke or have known medical risks.
What’s happening to our lungs? The answer lies in the way modern life has changed the air we breathe, the food we eat, and the way we live.
🏙️ 1. The Airborne Burden — Pollution and Particulates
Our lungs evolved to handle dust, pollen, and natural microbes — not microplastics, chemical fumes, or PM2.5 pollution.
The air quality crisis is now one of the leading environmental causes of death.
-
The World Bank estimates that air pollution costs the global economy over $8 trillion per year in healthcare and lost productivity.
-
PM2.5 particles, microscopic pollutants smaller than a red blood cell, penetrate deep into the lungs and bloodstream, causing inflammation that leads to asthma, COPD, and even heart disease.
-
In many major cities, breathing the air for one day is equivalent to smoking several cigarettes.
Even indoors, the air is far from safe. Household cleaners, synthetic fragrances, cooking oils, and mold release volatile organic compounds (VOCs) that quietly erode respiratory health.
This invisible assault is cumulative. Every breath counts — and so does every pollutant.
🍔 2. The Inflammation Diet — How Modern Food Fuels Lung Damage
Our lungs are deeply affected by what we eat. The connection between diet and respiratory health is one of medicine’s most overlooked frontiers.
The Western diet — heavy in sugar, refined oils, processed meats, and dairy — fuels systemic inflammation, which spreads to the delicate tissues of the lungs.
A 2023 study in The American Journal of Respiratory and Critical Care Medicine found that people who consumed high-sugar, low-antioxidant diets had 30% lower lung capacity than those who ate diets rich in fruits, vegetables, and omega-3 fats.
These inflammatory foods lead to oxidative stress, a buildup of harmful molecules that damage cellular structures in the respiratory tract.
Meanwhile, nutrient deficiencies — particularly vitamin D, magnesium, and zinc — weaken the immune system, leaving the lungs more vulnerable to infections and environmental toxins.
In short:
Our food can either stoke the fire of inflammation or cool it down.
Most modern diets are fanning the flames.
🧬 3. The Immune Overload — Autoimmunity and Viral Aftershocks
After decades of relative stability, we’re now seeing a rise in autoimmune and post-viral respiratory conditions.
COVID-19 reshaped the landscape of lung health — leaving behind millions of people struggling with long-term shortness of breath, fatigue, and inflammation long after the infection cleared.
These post-viral syndromes are partly caused by immune dysregulation: the body’s defense system becomes overactive and starts attacking its own tissues.
Similarly, autoimmune diseases like sarcoidosis, lupus, and rheumatoid arthritis often involve inflammatory reactions in the lungs.
The common denominator? A hyper-reactive immune system fueled by chronic stress, poor diet, and environmental exposure.
Our immune defenses are no longer at ease — they’re at war, often with ourselves.
🏠 4. The Indoor Generation — How Lifestyle Constricts the Lungs
We spend an average of 90% of our time indoors, often sitting for long periods in poorly ventilated spaces.
This combination — stagnant air, shallow breathing, and inactivity — weakens respiratory muscles and reduces lung elasticity.
Posture plays a major role.
When we hunch over screens, our diaphragm becomes compressed, and breathing shifts from the belly to the chest.
Over time, this leads to reduced oxygen exchange and reinforces a subtle sense of fatigue and anxiety.
Studies from the Cleveland Clinic show that sedentary lifestyles are directly linked to lower lung capacity, even in non-smokers.
The modern body is literally folding in on itself — and our breath is collapsing with it.
💊 5. The Chemical Cloud — From Cleaning Agents to Fragrances
Ironically, the very products marketed as “freshening” our environment often pollute it the most.
Household cleaners, air fresheners, scented candles, and even personal care items release volatile organic compounds (VOCs) that can irritate and inflame the respiratory tract.
Exposure to these substances can trigger headaches, coughing, wheezing, and, in sensitive individuals, chronic asthma-like symptoms.
A 2024 Environmental Health Perspectives review concluded that prolonged exposure to household VOCs increases the risk of developing asthma by up to 37%.
The average home now contains over 500 different synthetic chemicals, many untested for long-term respiratory safety.
The lungs, constantly filtering 10,000 liters of air daily, bear the brunt of this hidden chemical storm.
🧘 6. The Stress Epidemic — When Anxiety Steals Your Breath
There’s a reason we say, “Take a deep breath.”
Stress instantly changes how we breathe — shortening our inhalations and speeding up our exhalations.
This chronic tension keeps the body in a state of fight-or-flight, which elevates inflammation and tightens the respiratory muscles.
Over time, people under continuous stress may unconsciously adopt rapid, shallow breathing patterns that mirror anxiety itself.
Psychologists now call this the “stress-breath cycle” — a self-reinforcing loop where emotional strain alters breathing, and disordered breathing fuels more emotional strain.
Chronic stress doesn’t just affect the mind — it literally constricts the breath of life.
🌡️ 7. The Climate Factor — When the Planet Can’t Breathe Either
Global warming isn’t only a political or environmental issue — it’s a public health emergency.
Rising temperatures increase pollen seasons, wildfire frequency, and ozone levels, all of which aggravate respiratory symptoms.
Each degree of warming worsens air quality, increasing hospital admissions for asthma and COPD.
A Lancet Planetary Health study predicts that by 2050, climate-related respiratory illness will surpass malnutrition as a cause of early death in many regions.
When the planet struggles to breathe, so do we.
💬 A Crisis Hidden in Plain Sight
What makes this epidemic so insidious is that it rarely announces itself.
A cough here. A bit of shortness of breath there.
Most people adapt, ignoring the signs until a crisis forces them to pay attention.
We have normalized poor breathing and declining lung function — much like we’ve normalized fatigue, stress, and fast food.
The silent crisis of lung health is not just medical — it’s cultural.
It reflects the modern disconnection between how we live and what keeps us alive.
🌱 The Good News: It’s Reversible
The lungs are extraordinary healers. Within weeks of improving air quality, diet, and breathing patterns, measurable improvements occur in oxygen levels and inflammation markers.
New alveoli can form. Inflammation can subside. Breath capacity can expand.
Your body is constantly renewing itself — including your lungs.
The key lies in changing the internal and external environments that shape how they function.
In the chapters ahead, we’ll explore how to do just that — through nutrition, detoxification, movement, and conscious breathwork.
The air outside may be beyond your control.
But the air inside your body — that’s where your power begins.
🔑 Key Takeaway
The modern respiratory crisis is driven by pollution, diet, lifestyle, and stress — but it’s not irreversible. By addressing the root causes, you can transform your breath and your health.

by Rich Benvin | Oct 14, 2025 | Breathing, Lifestyle Medicine, Lung Health, Nutrition, Respiratory Health, Save Your Lungs
Chapter 1: The Miracle of Breathing
Breathe to Heal: How Nutrition and Lifestyle Can Save Your Lungs
You can go weeks without food, days without water — but only minutes without breath.
Breathing is the first thing you do when you enter this world, and the last thing you do when you leave it.
In between, it’s the rhythm that sustains every heartbeat, thought, and cell in your body.
Yet despite its power, breathing is the one thing we take most for granted.
We forget that each breath isn’t just air — it’s life in motion.
🫁 The Hidden Intelligence of Your Lungs
Your lungs are not just sacks of air. They are among the most complex and intelligent organs in your body — intricately designed to filter, exchange, and nourish.
Inside your chest are over 300 million alveoli, tiny balloon-like air sacs surrounded by an incredible network of capillaries.
Spread flat, this surface area equals about the size of a tennis court — all packed neatly inside your ribcage.
With each inhale, oxygen molecules travel down into these microscopic chambers, where they meet red blood cells and bind to hemoglobin.
In a split second, oxygen enters your bloodstream, fueling your brain, heart, and every living tissue in your body.
And on every exhale, carbon dioxide — a byproduct of metabolism — is released. This exchange happens roughly 25,000 times per day without you ever noticing.
When your lungs function well, they are a silent symphony of precision. But when inflammation, pollution, or stress disrupt that rhythm, the entire body feels it.
🧬 The Breath-Body Connection
Breathing is more than a mechanical process — it’s the translator between your body and your emotions.
When you’re anxious, your breath shortens.
When you’re calm, it deepens.
When you exercise, it accelerates to deliver more oxygen to your muscles.
This feedback loop between the lungs, brain, and nervous system is what scientists call the “respiratory-cardiac axis.”
-
When you inhale deeply, your heart rate slightly increases.
-
When you exhale slowly, it decreases.
This natural rhythm — known as respiratory sinus arrhythmia — synchronizes your heart and breath like partners in a dance.
It’s the biological foundation of calm.
That’s why techniques like meditation, yoga, and pranayama focus on lengthening the exhale — it directly activates the parasympathetic nervous system, your body’s built-in relaxation mode.
In other words: how you breathe determines how you feel.
🌿 Breathing Feeds Every Cell You Have
Oxygen is the currency of life. Every cell in your body depends on it to generate energy through a process called cellular respiration.
Without oxygen, your cells cannot produce adenosine triphosphate (ATP) — the molecule that powers all biological activity.
Even small reductions in oxygen levels can trigger fatigue, brain fog, and inflammation.
That’s why people who practice deep breathing often report higher energy, better focus, and emotional stability.
They’re not imagining it — they’re literally improving cellular efficiency.
But here’s what most people don’t realize:
Your ability to absorb and use oxygen isn’t fixed.
You can train your lungs, diaphragm, and circulation system to become stronger — just like a muscle.
Research from Harvard and the Cleveland Clinic shows that breathing exercises can:
-
Increase lung capacity by up to 20%
-
Lower resting heart rate and blood pressure
-
Reduce inflammatory markers (like CRP and IL-6)
-
Enhance immune cell activity
Breathing, in essence, is your most accessible form of medicine.
💨 The Breathing Spectrum: From Shallow to Superhuman
Most people breathe shallowly — drawing air into the upper chest instead of deep into the diaphragm.
This type of breathing, often caused by stress or posture, limits oxygen intake and activates the sympathetic “fight or flight” response.
Over time, chronic shallow breathing can lead to:
By contrast, diaphragmatic breathing — also called “belly breathing” — engages the largest muscle of respiration and fully expands the lungs.
It improves oxygen exchange, lymphatic flow, and even massages the organs of the abdomen.
Elite athletes, monks, and singers have long mastered this art — and studies show that it can extend life expectancy by improving cardiovascular and immune function.
Your breath, it turns out, is both a mirror of your current health and a lever for improving it.
🧠 The Mind in the Breath
Your breath also carries an emotional story.
When you’re angry, it’s rapid and hot.
When you’re grieving, it’s uneven and shallow.
When you’re peaceful, it’s smooth and rhythmic.
Every inhale and exhale is a message between the body and brain — a two-way conversation between physiology and psychology.
Neuroscientists have discovered that specific breathing rhythms stimulate regions of the brain linked to mood, attention, and memory.
Controlled breathing can even alter brainwave patterns, helping shift you from anxiety to clarity within minutes.
This is why breathwork is now being used in clinical settings to treat PTSD, depression, and panic disorders — it’s a tool that reconnects the nervous system with the body’s inner calm.
When you breathe consciously, you are no longer a victim of stress. You become its master.
🔬 Breathing and Inflammation: The New Frontier
In recent years, researchers have begun to understand how breathing directly influences inflammation and immunity.
Deep, rhythmic breathing increases levels of nitric oxide — a powerful molecule that opens blood vessels, improves circulation, and kills harmful pathogens in the respiratory tract.
At the same time, slow breathing reduces oxidative stress, which is one of the key drivers of chronic lung disease.
This connection explains why mindfulness, yoga, and meditation all have measurable effects on reducing inflammatory markers in clinical trials.
Your breath is not just a relaxation technique — it’s a biological signal that tells your immune system whether you are safe or in danger.
🌎 The Environmental Factor
Even the best lungs can’t thrive in toxic air.
From polluted cities to wildfire smoke, airborne particles now infiltrate every aspect of modern life. These microscopic invaders — PM2.5, ozone, and nitrogen oxides — trigger inflammation, constrict airways, and increase susceptibility to infection.
This makes it even more essential to strengthen the lungs internally — through antioxidant nutrition, hydration, and mindful breathing practices that support cellular repair.
As the world’s air quality declines, individual lung care becomes a global act of self-preservation.
💡 Key Takeaway: Your Breath Is Your Baseline
Every breath you take carries information about your body’s balance.
If you breathe shallowly, rapidly, or unconsciously — your body interprets life as a threat.
If you breathe deeply, slowly, and rhythmically — your body interprets life as safe.
Your lungs don’t just keep you alive — they teach you how to live.
By understanding and honoring the miracle of breathing, you reclaim control over your most essential function and begin the healing process from within.
🌤️ In the Next Chapter…
We’ll explore why respiratory diseases are skyrocketing across the globe — the environmental, nutritional, and emotional factors driving the modern lung health crisis — and what science reveals about how to reverse it.